Fighting Back: Unmasking SARS-CoV-2 PLpro's Drug Resistance Hotspots
- Ray Sullivan

- Jul 17, 2025
- 4 min read

The global battle against SARS-CoV-2, the virus behind COVID-19, continues to evolve. While the pandemic may be winding down, the virus and its capacity to mutate remain a significant challenge to public health. A key weapon in our antiviral arsenal is targeting viral proteases, enzymes essential for the virus's life cycle. Among these, the SARS-CoV-2 papain-like protease (PLpro) stands out. Not only does PLpro play a pivotal role in processing viral polyproteins, enabling the virus to replicate, but it also helps the virus evade our immune responses. This dual functionality makes PLpro a highly promising, albeit challenging, drug target.
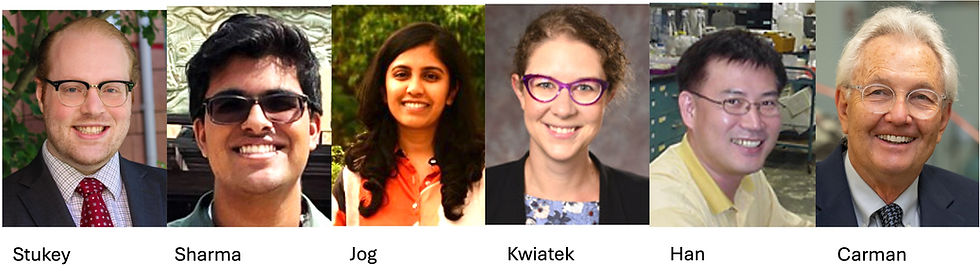
Recent breakthroughs have led to the development of first-in-class PLpro inhibitors like Jun12682 (Rutgers & Oklahoma State) and PF-07957472 (Pfizer), which have shown potent antiviral efficacy in mouse models. However, the virus's high mutation rate means that drug resistance is an inevitable concern, as seen with other approved antivirals targeting different viral proteins. Understanding how SARS-CoV-2 might develop resistance to these new PLpro inhibitors is crucial for designing future treatments.
The team that designed Jun12682, Jun Wang’s Lab at Rutgers and Xufang Deng’s Lab at Oklahoma State, along with colleagues from the National and Kapodistrian University of Athens, delved deep into this challenge, systematically identifying naturally occurring mutations in PLpro that could lead to drug resistance against Jun12682. They employed two independent and complementary approaches:
They analyzed existing SARS-CoV-2 genetic sequences in the GISAID database to pinpoint high-frequency mutations at residues known to interact directly with Jun12682.
They continuously exposed live SARS-CoV-2 viruses to increasing concentrations of Jun12682 in cell culture, mimicking the evolutionary pressure the virus might face during treatment. This method helps validate the physiological relevance of identified mutations.
For a mutation to be considered a "physiologically relevant drug-resistant mutant," it had to meet two critical criteria: it must maintain comparable enzymatic activity as the wild-type PLpro (meaning it doesn't significantly impair viral function), and it must show a significant increase (more than 10-fold) in drug resistance (Ki value) compared to the wild-type.
The study conclusively identified E167, Y268, and Q269 as key drug-resistance hotspots for PLpro inhibitors that bind to the BL2 loop and groove region, such as Jun12682 and PF-07957472. Molecular dynamics simulations further illuminated why these mutations confer resistance: they weaken crucial interactions between the inhibitor and the enzyme.
Here's a breakdown of the most impactful mutations:
E167 Mutations: The amino acid E167 forms a vital electrostatic interaction with Jun12682. Mutations like E167G, E167K, E167A, E167S, and E167V caused significant resistance, with Ki values increasing by more than 24-fold, and in some cases, over 130-fold, while maintaining normal enzymatic activity. The E167G mutation, in particular, was also identified in the viral passage experiments. Molecular simulations revealed that the E167G mutation leads to missing hydrogen bonding interactions with key residues, contributing to reduced drug binding.
Y268 Mutations: Y268 is critical for drug binding, typically forming a π-π stacking interaction with Jun12682. The common Y268H mutation showed substantial cross-resistance to Jun12682, PF-07957472, and even GRL0617, with Ki increases of 41-fold, 75-fold, and 22-fold respectively, all while maintaining enzymatic activity comparable to the wild-type. Another mutation, Y268N, exhibited even higher levels of cross-resistance (e.g., >385-fold for Jun12682). MD simulations showed that in the Y268H mutant, the π-π stacking interaction is lost.
Q269 Mutations: Q269 forms a hydrogen bond with Jun12682. The Q269H mutation demonstrated comparable enzymatic activity to wild-type and conferred significant resistance to both Jun12682 and PF-07957472, increasing Ki values by more than 13-fold. This mutation rapidly emerged and became dominant in the viral passage experiments, validating its physiological relevance.

Interestingly, the serial viral passage experiments also identified allosteric mutations at residues V98, L152, and T168. While these sites are not directly involved in drug binding (being more than 8Å away from the inhibitor), they do not confer drug resistance on their own. However, when combined with the E167G or Q269H mutations, they significantly enhance the degree of drug resistance. This suggests a complex interplay where mutations outside the direct binding pocket can still impact drug efficacy.
This study provides invaluable insights into the genetic barrier to drug resistance for PLpro inhibitors. The findings suggest that SARS-CoV-2 variants encoding mutations at E167, Y268, and Q269 are likely to be resistant to inhibitors like Jun12682 and PF-07957472. Therefore, monitoring circulating SARS-CoV-2 strains for these specific mutations is crucial for public health surveillance.
The research also offers a clear roadmap for designing next-generation PLpro inhibitors that can circumvent these resistance mechanisms. For instance, future inhibitors could be designed to avoid forming electrostatic interactions with E167 or modifying the linker region to bypass Q269 mutations. However, such modifications would need careful consideration to ensure they don't compromise the drug's binding affinity and antiviral activity.
It's important to note that these findings are specific to SARS-CoV-2 and PLpro inhibitors that target the BL2 loop and groove region. The continuous evolution of SARS-CoV-2 underscores the importance of ongoing research into novel antiviral strategies and understanding resistance mechanisms to stay ahead of the virus.
Tan H, Zhang Q, Georgiou K, Zhang S, Li K, Lambrinidis G, Kolocouris A, Deng X, Wang J. Identification of naturally occurring drug-resistant mutations of SARS-CoV-2 papain-like protease. Nat Commun. 2025 May 16;16(1):4548. doi: 10.1038/s41467-025-59922-9. PMID: 40379662; PMCID: PMC12084387.









Comments