A Game-Changer for HIV Prevention? Weekly Islatravir Shows Promise for Post-Exposure Prophylaxis
- Ray Sullivan

- Jul 23
- 4 min read
Imagine a single pill that could prevent HIV infection after a potential exposure, removing the burden of a 28-day daily regimen. Islatravir is an investigational drug developed by Merck for the treatment of HIV infection. Scientists from Merck (Rahway, NJ), Tulane, and the Aaron Diamond AIDS Research Center recently published results that offer exciting insights into this possibility, highlighting the potential of islatravir as a simplified post-exposure prophylaxis.
Currently, the standard of care for HIV Type 1 post-exposure prophylaxis involves taking a combination of antiretroviral agents daily for 28 days after exposure. This regimen needs to be started ideally within 24 hours, and no later than 72 hours, after potential HIV exposure to be most effective. While effective, the long duration and daily adherence requirements can be challenging for individuals. This underscores the critical need for more convenient and accessible post-exposure prophylaxis options.
Islatravir is a powerful new-generation nucleoside reverse transcriptase translocation inhibitor. It is highly effective against both wild-type HIV Type 1 and drug-resistant variants, showing no known cross-resistance with other antiretroviral classes. What makes islatravir particularly appealing for post-exposure prophylaxis is its sub-nanomolar potency, long half-life, and broad tissue distribution, which make it suitable for less frequent dosing, including weekly administration. Once inside target cells, islatravir is quickly converted into its active form, islatravir triphosphate, which then works to inhibit HIV Type 1 reverse transcriptase activity.
Researchers conducted a comprehensive study using a simian immunodeficiency virus (SIV) rhesus macaque intravenous challenge model to evaluate islatravir's efficacy as post-exposure prophylaxis. Twelve rhesus macaques were challenged with SIV via intravenous administration. After 24 hours, six animals received weekly oral doses of islatravir, while six served as untreated controls. The study was conducted in four stages, progressively reducing the number of weekly islatravir doses administered after exposure:
Stage 1: Four weekly oral doses.
Stage 2: Three weekly oral doses.
Stage 3: Two weekly oral doses.
Stage 4: A single oral dose.
In each stage, uninfected animals from the treated group of the previous stage were re-challenged and treated, then monitored for simian immunodeficiency virus infection for 7 weeks after their last islatravir dose. Infection was monitored through plasma viral RNA, proviral DNA amplification, and virus-specific antibody responses. Islatravir concentrations in plasma and islatravir triphosphate levels in peripheral blood mononuclear cells were also measured.
The results were highly encouraging:
All untreated control animals became viraemic (detectable virus in blood) within 7 days after SIV intravenous challenge. In stark contrast, all six islatravir-treated animals were completely protected in stages 1, 2, and 3 (receiving 4, 3, or 2 weekly doses, respectively). This complete protection meant no observed viraemia above the lower limit of detection, and no detectable proviral DNA or SIV antibodies. This protection correlated with sustained islatravir triphosphate levels.
Near Protection with a Single Dose: In stage 4, where animals received only a single oral dose of islatravir, four out of six animals were still protected, demonstrating significant efficacy. Two animals did become infected, with viraemia observed at day 14 and day 49, respectively. Notably, both of these infected animals had unquantifiable islatravir triphosphate levels on the day viraemia was observed, suggesting a correlation between sustained drug levels and protection. Overall, the data indicated a greater than or equal to 39-fold lower risk of infection in islatravir-treated animals compared to controls.
While two weekly doses were necessary for complete protection in the macaque model, a crucial difference exists: the terminal half-life of islatravir triphosphate in human peripheral blood mononuclear cells is approximately 190 hours, which is substantially longer than the approximately 50 hours observed in macaque peripheral blood mononuclear cells. This means that in humans, islatravir triphosphate levels are maintained at higher concentrations for a longer duration.
Based on this pharmacokinetic difference, the study suggests that a single oral dose of islatravir given as post-exposure prophylaxis within 24 hours of HIV exposure could potentially provide a protective effect in humans.
This research strongly supports further investigation into long-acting oral nucleoside reverse transcriptase translocation inhibitors like islatravir for simplified HIV Type 1 post-exposure prophylaxis in humans. The potential benefits of a single-dose oral post-exposure prophylaxis are immense: it would address the need for urgent initiation, eliminate the adherence challenges of a 28-day regimen, and islatravir's attributes of being well-tolerated with minimal drug-drug interactions make it highly suitable for diverse populations.
While the clinical development of once-monthly oral islatravir for pre-exposure prophylaxis was paused due to dose-dependent lymphocyte count decreases at higher doses, it is important to note that islatravir continues to be investigated for HIV Type 1 treatment at lower doses (0.25 milligrams daily and 2 milligrams weekly) where lymphocyte decreases have not been observed. Furthermore, a novel nucleoside reverse transcriptase translocation inhibitor called MK-8527 is currently in clinical development for monthly oral HIV Type 1 prophylaxis, with promising early results.
The findings from this macaque study bring us a significant step closer to a more accessible and effective post-exposure prophylaxis, potentially transforming how we prevent HIV acquisition globally.
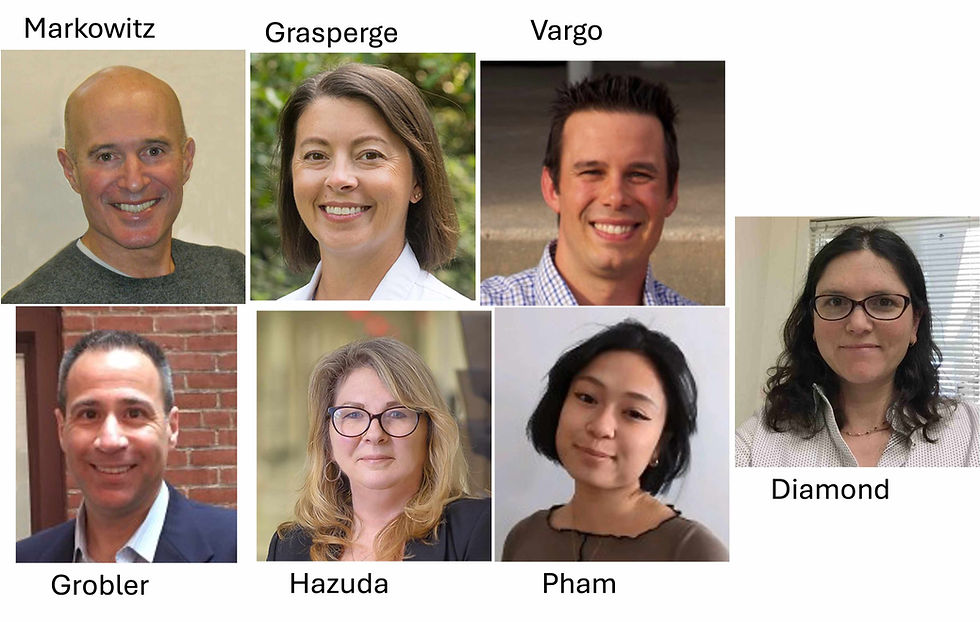
Markowitz M, Gettie A, St Bernard L, Grasperge B, Vargo R, Pham M, Fillgrove K, Dube N, Diamond TL, Hazuda DJ, Grobler JA. Effectiveness of islatravir post-exposure prophylaxis after intravenous challenge with simian immunodeficiency virus in rhesus macaques. J Int AIDS Soc. 2025 Jun;28(6):e26507. doi: 10.1002/jia2.26507. PMID: 40534150; PMCID: PMC12177105.










Comments